
A deer tick, also known as a blacklegged tick, the species that transmits Lyme disease in the Eastern U.S.
Photo by Jerry Kirkhart.
If you like taking long walks in the Eastern woods with your dog, you should be sure your furry friend is vaccinated against tick-borne Lyme disease. I would say you should vaccinate yourself, too, but currently humans don’t have that option.
That may change if Valneva SE, a pharmaceutical company based in France, is able to secure regulatory approval. But regulatory scrutiny may not be the vaccine’s only hurdle. Some patient advocacy groups are also suspicious, or even hostile, to the idea of a new vaccine, The Wall Street Journal recently reported.
Valneva announced Phase 1 clinical trial results in March; Phase 2 trials are set to begin later this year. The U.S. Food and Drug Administration has granted the vaccine fast-track status, though it is still at least five years away from commercial production. Unlike an earlier vaccine, Lymerix, the new version protects against six strains of the disease and does not incorporate a gene sequence that some scientific papers had tied to arthritis. Lymerix received FDA approval in 1998, but its maker voluntarily discontinued it in 2002.
I would have thought that advocacy groups that deal with Lyme disease would be excited at any prospect for a new vaccine – or even for the commercial revival of an old vaccine that has been taken off the market for humans. Lymerix’s story may shed at least some light on this seeming paradox.
What happened to Lymerix is, like many aspects of Lyme disease, the subject of some controversy. GlaxoSmithKline developed the Lymerix vaccine in the late 1990s and reported a 78 percent efficacy rate after three doses. A major class-action lawsuit, however, alleged that Lymerix caused serious side effects, including arthritis. The litigation was settled in 2003, but GSK voluntarily discontinued Lymerix a year earlier. A spokeswoman for the company told The Wall Street Journal that it pulled the vaccine due to low demand. The Journal also reported that no evidence emerged that definitively tied Lymerix to arthritis, though some scientific papers had identified a gene sequence in Lymerix as potentially related to the disease.
The low demand cited by GSK had several causes, and their relative importance depends on whom you ask. Part of the problem was practical: The vaccine required three shots over the course of a year, plus periodic booster shots, and it did not become effective right away. It was also not approved for inoculating anyone under 15 years old. (The vaccine was never tested in children.) Health insurance companies were not required to cover Lymerix’s cost, about $50 per dose, a factor which is never helpful to a vaccine’s widespread adoption. And, of course, there were the patients convinced of the vaccine’s potentially serious side effects, such as the plaintiffs in the class-action suits, despite investigations into the claims by the FDA and the Centers for Disease Control that came up clean.
Anti-vaccination positions are, unfortunately, neither new nor uncommon. It is likely, therefore, that some of the pushback simply reflected wider distrust of vaccines in the general population. But Lymerix in particular may have suffered in the context of broader tensions between patients and medical professionals about Lyme disease diagnosis and treatment.
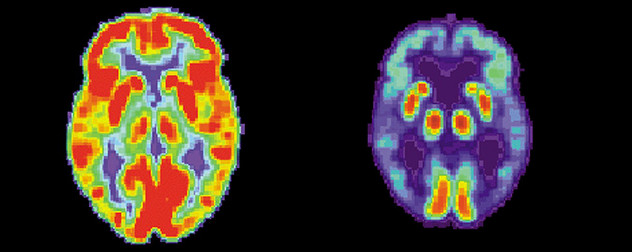
Controversy aside, Lyme can be a painful and sometimes debilitating disease. People who get antibiotics in the early stages usually make a full recovery, but patients who do not receive treatment until later stages can suffer at length due to long-term damage to their joints or nervous systems. Lyme disease is endemic to the Northeast, and spreading along with the ticks that cause it. These are facts upon which everyone can agree.
Patient groups have persistently argued, however, that Lyme disease is poorly understood and poorly diagnosed by many physicians. Part of this could be due to the fact that, until recently, it was relatively rare; reported cases tripled between 2004 and 2016. Belated diagnosis would be a problem with any serious malady, but there is a significant difference in prognosis for patients who receive treatments soon after infection and for those who do not receive antibiotics until later stages of the disease.
Some patients also experience fatigue, pain and muscle aches that certain physicians describe as “post Lyme disease syndrome.” Arguments over whether Lyme is a chronic condition are often advocates’ principle focus. Because there is no consensus on “chronic” Lyme disease’s prevalence, treatment or even its diagnostic criteria, some physicians are openly dismissive of post Lyme disease syndrome’s very existence, while others are willing to use the label but can offer no therapeutic options. Still others recommend long-term antibiotic use despite the very real risks of such treatments. For patients experiencing chronic pain or neurological symptoms, this situation is doubtless incredibly frustrating. But it seems that it has created a subset of individuals who distrust anything Lyme-related emerging from the medical establishment.
Lorraine Johnson, the CEO of the nonprofit advocacy group LymeDisease.org, told The Wall Street Journal that her community worried that Valneva was not displaying sufficient transparency in the vaccine development process. “The last Lyme vaccine that came out had significant safety concerns,” Johnson said. Patricia Smith, who is the president of the nonprofit group Lyme Disease Association Inc., felt there was insufficient research as to what went wrong with Lymerix, and expressed concerns about potential similarities between the new vaccine and the old one.
I can’t say exactly what is on the minds of these self-selected patient advocates. They seem to see themselves, rather than the FDA and other regulators, as the properly empowered gatekeepers. Assuming they are acting in good faith, perhaps longstanding frustration with the treatment of Lyme disease has led them to distrust pharmaceutical companies and regulators.
In a column for LymeDisease.org, Dorothy Kupcha Leland reacted to The Wall Street Journal’s coverage by both praising the author for speaking to Lyme advocacy groups and criticizing her characterization of such groups as a “powerful lobby.” She also describes a “disinformation campaign” about Lymerix and repeats a widely spread report that Phase IV clinical trial data was never released. However, in an article for Forbes, immunologist Tirumalai Kamala cited that trial data, which showed an equal arthritis rate in vaccinated individuals and the control group. Gregory Poland, a vaccinologist at the Mayo Clinic, also noted that there were no differences in significant adverse reactions between the groups in a 2011 article supporting the reintroduction of a Lyme vaccine. (This was also true of the wider population receiving the vaccine outside a trial setting.)
Some pharmaceutical companies have indeed made high-profile moves warranting scrutiny and criticism, but I cannot see any evidence that Valneva is proceeding in bad faith. On the contrary, while Lyme disease is serious, the population it affects is relatively small, so many drug companies have previously said that they simply aren’t interested in pursuing research when vaccines for other conditions are more likely to be profitable. A group of biotech professionals have also formed an alliance to bring back Lymerix as a generic product and distribute it as a nonprofit in an effort to reduce infection rates, undercutting the idea that the medical community’s interest in pushing a Lyme vaccine is a simple cash grab.
An effective vaccine need not be a perfect vaccine. It need not address all the other diseases that ticks can spread, nor necessarily every strain of Lyme, although of course the more strains, the better. Almost anything would be better than what we have now, which is nothing except a lot of deer and even more ticks.











July 18, 2018 - 10:11 pm
An earlier polio vaccine did not include enough variation, and people still got polio. This resulted in an apology and hard work to produce a better vaccine. No one accused the victims of polio of being anti vaccine. The fact is that there were published papers showing why some people who got the lyme vaccine had adverse consequences. If this had been admitted, and the flaws fixed, you would not now have people with lyme being scared of a new vaccine.
Do you really think that people will be forgiving about getting a flawed vaccine without enough coverage of variation? Will they say, oh so what I got lyme but I still think this is a good vaccine? Unlikely. And what is likely is that the vaccine will give people a false sense of security. Ticks can carry more than a dozen diseases. You are vaccinated against some strains of lyme bacteria, and against no other diseases. This is a pretty small step toward having protection in that walk in the woods.
Lyme patients do not have power. They do not have health. Frequently they cannot work, cannot get adequate treatment, are assumed to be cured when given treatment that might work for an early case, but not for late stage cases. The power is in the medical establishment, the government health agencies, the pharmaceutical industry, and the insurance industry. Let’s not pretend that it is an equal match.